Introduction: The Technological Change of Patient Care
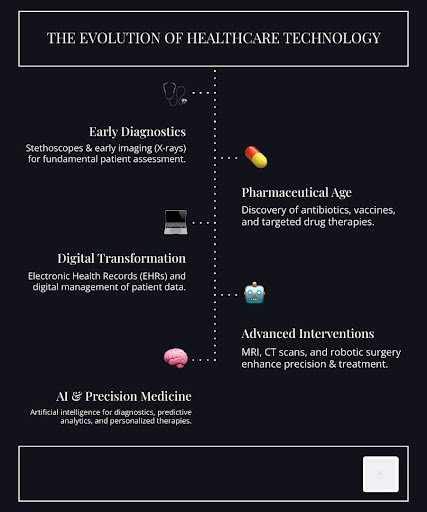
Healthcare is undergoing a profound change, driven by relentless technological innovation. The core mission of medicine—to heal and protect—is being redefined by advancements that promise not only to improve treatment but also to enhance patient safety fundamentally. For too long, preventable errors and inefficiencies have plagued healthcare systems. Startling statistics from studies like the 1991 Harvard Medical Practice Study, which reported between 44,000 and 98,000 preventable deaths per year in hospitals, underscore the critical need for change. Technology offers a powerful antidote, moving us towards a future where care is not just effective, but inherently safer.
This digital revolution spans every facet of the healthcare ecosystem, from the diagnostic tools that uncover hidden ailments to the sophisticated systems that manage patient records and streamline hospital operations. We are witnessing a shift from reactive treatment to proactive, personalized care, where data-driven insights and advanced devices empower both clinicians and patients. This comprehensive guide will examine how cutting-edge healthcare technology is transforming the landscape of patient safety, with a focus on its impact on healing, infection control, and the delivery of essential medical supplies. We will delve into the specific innovations that are making a tangible difference, examine the challenges that must be overcome, and look ahead to the exciting future of technologically advanced patient care.
A New Era of Healing: How Technology Accelerates Recovery
The journey of healing, traditionally reliant on human intervention and pharmaceutical solutions, is being revolutionized by technologies that accelerate recovery, minimize discomfort, and improve long-term outcomes. These innovations are critical for patient safety, reducing the risks associated with prolonged recovery periods and enhancing the body’s natural restorative processes.
The Role of Far-Infrared Healthcare Technology in Healing
One promising area in non-invasive therapy is the application of far-infrared (FIR) technology. Unlike traditional heating methods, FIR penetrates deeper into tissues, promoting cellular regeneration, increasing localized blood flow, and reducing inflammation without direct contact or excessive heat. This gentle yet effective approach is gaining traction in regenerative medicine, offering a non-pharmacological pathway to recovery.
For patients recovering from surgery or managing chronic conditions, therapies that enhance the body’s healing capabilities can significantly improve safety by reducing reliance on medications with potential side effects and accelerating the recovery process. Devices that leverage advanced far-infrared technology, such as the innovative SemiCera® healthcare technology, are designed to support these natural processes, offering a comfortable and effective solution for post-surgical recovery and overall well-being. By stimulating cellular activity and improving circulation, such technologies contribute to faster tissue repair and reduced pain, making the healing process safer and more efficient.

Advanced Wound and Soft Tissue Injury Management
Wound care, particularly for chronic wounds and complex soft tissue injuries, has long been a significant challenge in healthcare, often leading to prolonged hospital stays and increased risk of infection. However, a new generation of healthcare technology is transforming this field, offering advanced solutions for faster and more effective healing.
Here are some key technologies improving wound care:
- Smart Bandages: These advanced dressings incorporate sensors that monitor wound conditions in real-time, detecting changes in temperature, pH, and moisture levels, as well as the presence of infection. They can release medication automatically, providing targeted and personalized treatment.
- 3D Printing for Skin Grafts: Custom-printed skin grafts, custom to a patient’s specific wound size and shape, are improving outcomes for severe burns and chronic ulcers. This technology minimizes scarring and accelerates healing by providing a precise biological match.
- Bioprinting: Moving beyond simple grafts, bioprinting allows for the creation of complex tissues and organs using a patient’s own cells. While still mainly in the research stage, its potential for personalized medicine in wound repair is immense, offering solutions for even the most challenging injuries.
- Negative Pressure Wound Therapy (NPWT): This established technology uses a vacuum pump to draw fluid from the wound, promoting blood flow and tissue growth, and reducing bacterial colonization. Modern NPWT devices are smaller, more portable, and often integrated with digital monitoring capabilities.
- Growth Factors and Biologics: Advanced biologic therapies, including cells, proteins, peptides, and genes, are utilized to stimulate healing at the molecular level. While often expensive, with costs ranging from $10 to $100 million for development and regulatory approval, they offer targeted interventions for complex wounds.
The integration of these technologies into clinical practice holds the promise of significantly reducing complications, improving patient comfort, and ensuring a safer, more predictable healing journey for individuals with chronic wounds and soft tissue injuries.
Combating Infections: Automated Disinfection and Sterilization
Hospital-acquired infections (HAIs) represent a persistent and dangerous threat to patient safety, contributing to extended hospital stays, increased healthcare costs, and, tragically, preventable deaths. Traditional manual cleaning methods, while essential, have inherent limitations. The advent of automated disinfection systems and robust supply chain integrity measures is pivotal in creating safer healthcare environments.
The Rise of Automated Disinfection Systems
Innovative automated disinfection technologies are bolstering the fight against HAIs. These systems address the shortcomings of manual cleaning by ensuring consistent and thorough decontamination of surfaces, even in hard-to-reach areas. UV-C light technology, for instance, uses specific wavelengths of ultraviolet light to destroy the DNA and RNA of bacteria, viruses, and other pathogens, rendering them unable to replicate.
Smart hospitals are increasingly deploying robotic solutions equipped with UV-C light or hydrogen peroxide vapor to disinfect patient rooms, operating theaters, and common areas. These autonomous systems can operate during off-peak hours, providing a layer of infection control that complements human efforts. For instance, specialized automated disinfection solutions, such as those offered by MicroLumix automated healthcare technology, are designed to deliver precise and effective pathogen elimination, significantly reducing the environmental bioburden. This proactive approach to infection control is a cornerstone of modern patient safety initiatives, helping to protect vulnerable patients from potentially life-threatening infections.

Sterilization and Supply Chain Integrity
Beyond environmental disinfection, ensuring the sterility of surgical instruments and the integrity of medical supply chains is paramount. Surgical tool sterilization processes have become increasingly sophisticated, utilizing high-temperature steam, chemical sterilants, and radiation to eliminate all microbial life. However, the challenge extends to tracking these items and ensuring the authenticity and safety of all medical products entering the healthcare system.
Blockchain technology is emerging as a powerful solution for enhancing data security and privacy within the medical supply chain. By creating decentralized and tamper-proof records of patient information, manufacturing details, and distribution logs, blockchain can significantly reduce the risk of data breaches and ensure the provenance of drugs and devices. This digital ledger technology enables select participants to securely share and update critical data, making it a vital component of the industry’s infrastructure for safeguarding patient information and ensuring that only legitimate, high-quality medical supplies reach patients. This robust data security and transparency are crucial for preventing counterfeit products from entering the market and for quickly tracing any contaminated or faulty items, protecting patient health at every step.
Improving Access and Outcomes with Durable Healthcare Technology
Ensuring patients have consistent access to the necessary tools for their care, both within medical facilities and in their homes, is a fundamental aspect of patient safety. Durable healthcare technology plays a crucial role in extending care beyond hospital walls, fostering greater patient autonomy, and maintaining continuity of treatment.
Modernizing Durable Medical Equipment (DME)
Durable Medical Equipment (DME) has traditionally encompassed items like wheelchairs, oxygen tanks, and hospital beds. However, with advancements in digital health, the scope of DME is rapidly expanding to include sophisticated devices that empower patients and integrate seamlessly with telehealth services. Remote patient monitoring (RPM) is a key component of this modernization, enabling healthcare providers to continuously track vital signs, glucose levels, heart rate, and other critical health data remotely.
Wearable sensors and smart devices, which are quickly evolving to provide nurses and other members of the healthcare team with more detailed data, enable real-time insights into a patient’s condition, facilitating proactive interventions and personalized treatment adjustments. This not only improves patient outcomes but also reduces the need for frequent in-person visits, enhancing convenience and accessibility, especially for those in remote areas or with mobility challenges. Companies specializing in Durable healthcare technology are at the forefront of this evolution, offering advanced solutions that support home healthcare and chronic disease management, ultimately leading to greater patient empowerment and a safer, more connected care experience.
On-Demand Medical Devices and Customization
The ability to rapidly produce and customize medical devices is another significant stride in enhancing patient safety and treatment efficacy. 3D printing technology has emerged as a game-changer in this regard, moving beyond prototyping to create functional and patient-specific medical tools and implants.
The number of hospitals with 3D printing facilities has increased significantly in recent years, reflecting the growing recognition of the benefits of this technology. This technology allows for:
- Customized Prosthetics: Creating prosthetics that perfectly fit an individual’s anatomy, improving comfort, function, and acceptance.
- Patient-Specific Implants: Producing implants for orthopedic, dental, and craniofacial surgeries that are precisely matched to the patient’s unique biological structure, leading to better surgical outcomes and reduced complications.
- 3D Printed Surgical Tools: Manufacturing specialized surgical guides and instruments that improve precision during complex procedures, potentially reducing surgical time and improving accuracy.
This level of customization not only improves the fit and function of medical devices but also has the potential to reduce manufacturing costs and accelerate the availability of critical supplies. By tailoring devices to individual patient needs, we can minimize risks, optimize recovery, and ensure that every patient receives the most appropriate and effective care possible.
Overcoming Challenges in Adopting New Healthcare Technology
While the promise of healthcare technology is immense, its widespread adoption and effective integration are not without significant problems. Addressing these challenges is crucial to ensuring that innovations truly contribute to patient safety and equitable access to care.
Regulatory Oversight and Financial Problems
The path from a novel idea to a widely used medical technology is fraught with regulatory complexities and substantial financial investment. The FDA, for instance, has two primary processes for evaluating new healthcare technology: the 510(k) or pre-market notification process for devices similar to existing ones, and the more rigorous pre-market approval (PMA) process for entirely new devices. The PMA process, which often takes 4–5 years to complete and is very expensive, requires extensive clinical trials.
The cost of developing new technologies is staggering. For example, a new knee implant system can require an investment of $10–20 million and take 2–4 years before market availability. Orthobiologics, including cells, proteins, and genes, can incur development costs of $10–100 million, with an additional $10 million for regulatory approval. These high costs are often passed on to consumers, contributing to the rising costs of healthcare.
Furthermore, the influence of direct-to-consumer advertising (DTCA) by device manufacturers, which cost approximately $600 million to $2.5 billion between 1996 and 2000, can create demand for new technologies before their long-term efficacy and cost-effectiveness are fully established. This raises questions about informed patient choice and the ethical responsibilities of industry. Navigating these financial and regulatory landscapes requires significant capital, strategic planning, and a commitment to transparency.
Assessing the Efficacy of New Healthcare Technology
Beyond regulatory approval, the actual impact of new healthcare technologies must be rigorously assessed in terms of efficacy, safety, and cost-effectiveness. This is the role of Healthcare Technology Assessment (HTA), a multidisciplinary evaluation that considers clinical benefits, risks, feasibility, and economic implications. Despite its critical importance, the cost of HTA is often less than 0.3% of the total amount spent on healthcare, highlighting a potential underinvestment in this vital area.
Methods for HTA include prospective randomized trials, which are considered the most powerful for establishing efficacy, as well as case series, epidemiological studies, and clinical registries. Registries, such as the highly successful Swedish hip registry, have demonstrated their value by significantly reducing the rate of revision surgery for total hip arthroplasty. Such data-driven approaches provide invaluable post-market surveillance, identifying long-term complications and informing best practices.
However, the adoption of new technologies also introduces significant challenges related to data privacy and cybersecurity. As more patient data is digitized and shared across interconnected systems, robust protections are essential to ensure HIPAA compliance and prevent breaches. The ethical implications of AI algorithms, including potential biases and the need for transparency, also require careful consideration. A comprehensive approach to HTA, coupled with strong ethical frameworks and cybersecurity measures, is vital to harness the full potential of healthcare technology while safeguarding patient trust and well-being.
Conclusion: The Future of Patient Safety is Technological
The rapid evolution of healthcare technology is undeniably reshaping patient safety, offering unprecedented opportunities to improve healing, prevent infections, and improve access to care. From advanced far-infrared therapies that promote cellular regeneration to automated disinfection systems that sterilize hospital environments, and from personalized 3D-printed implants to remote patient monitoring, we are witnessing a paradigm shift in how healthcare is delivered.
These innovations are not merely incremental improvements; they represent fundamental changes that empower patients, enhance treatment precision, and streamline operational efficiencies. AI and machine learning technologies, for instance, are becoming critical in the modern healthcare landscape, assisting in diagnostics, accelerating drug findy, and even reducing the documentation burden on healthcare professionals. Emerging trends, such as generative AI, nanotechnology, and digital therapeutics, promise even more transformative impacts, offering new avenues for personalized treatment and proactive health management.
However, realizing this future demands a collaborative and conscientious effort. We must navigate the complex terrain of regulatory oversight, address the financial implications of high development costs, and rigorously assess the efficacy and safety of new technologies through robust Healthcare Technology Assessment (HTA) processes. Cybersecurity, data privacy, and ethical considerations must remain at the forefront of every technological advancement.
The journey towards a safer, more effective healthcare system is a shared responsibility. Physicians, industry leaders, and regulatory bodies, such as the FDA, must work in concert to ensure that innovation serves the ultimate goal: prioritizing patient well-being. By embracing evidence-based adoption, fostering interoperability, and proactively addressing challenges, we can collectively open up the full potential of healthcare technology to create a future where patient safety is not just an aspiration, but a consistent reality.

