Despite the universal need for medical attention, countless individuals encounter formidable obstacles when attempting to access healthcare services. These roadblocks are multifaceted, stemming from financial constraints, geographic isolation, physical limitations, and communication gaps. Understanding these barriers is the first step toward dismantling them and building a truly inclusive healthcare system.
Financial and Geographic Problems
One of the most significant problems to accessible healthcare is financial. The cost of medical care in many regions, particularly in the United States, can be prohibitive. We know that about 1 in 10 people in the United States don’t have health insurance, and nearly 27 million Americans were uninsured in 2020. This lack of coverage often leads to delayed or forgone care, as individuals simply cannot afford the necessary treatments or preventive services. Even for those with insurance, high deductibles, co-pays, and out-of-pocket maximums can create substantial financial burdens, forcing difficult choices between health and other essential needs.
Beyond personal finances, geographic disparities also play a crucial role. Approximately 20% of Americans live in rural regions, where healthcare resources are often severely limited. These areas frequently face shortages of healthcare professionals, specialists, and even basic medical facilities. Long travel distances to the nearest clinic or hospital, coupled with inadequate public transportation options, make it incredibly difficult for rural residents to access timely care. This creates what are often referred to as “healthcare deserts,” where essential services are simply out of reach.
Moreover, cultural and language barriers can exacerbate these issues. Patients from diverse backgrounds may struggle to find providers who understand their cultural context or speak their native language, leading to misunderstandings, mistrust, and ultimately, poorer health outcomes. Addressing these complex needs requires a nuanced approach, often involving providers specializing in Culturally accessible healthcare to ensure that care is not only physically available but also culturally competent and respectful.
Physical and Communication Barriers to Accessible Healthcare
Beyond finances and geography, physical barriers within healthcare facilities themselves prevent many individuals, especially those with disabilities, from receiving adequate care. Imagine trying to steer a clinic with narrow doorways, no ramps, or inaccessible restrooms if you use a wheelchair. These are daily realities for many. We know that approximately 25% of U.S. adults have at least one disability, yet many healthcare settings are not designed with them in mind.
A stark statistic highlights this issue: among physicians seeing patients with significant mobility limitations, only 40 percent always or usually used accessible exam tables or chairs. This means a majority of patients with mobility challenges may struggle to even get onto an exam table, compromising the quality and dignity of their care. These physical impediments extend to medical equipment like mammography machines or scales, which are often not adjustable or accessible for individuals with mobility disabilities.
Equally critical are communication barriers. For patients with hearing, vision, speech, or cognitive disabilities, effective communication with healthcare providers can be a significant challenge. Without qualified sign language interpreters, large print materials, Braille, or simplified explanations, vital medical information can be lost, leading to misdiagnoses or ineffective treatment plans. The digital divide also plays a part, as not all patients have access to or proficiency with online tools, further complicating communication and access to information.
Bridging the Gap: The Role of Technology in Accessible Healthcare
Technology has emerged as a powerful tool in dismantling many of these traditional barriers, offering innovative solutions to make healthcare more accessible than ever before. From virtual consultations to remote monitoring, digital advancements are reshaping how we deliver and receive medical services.

The Rise of Telemedicine and Remote Care
Perhaps the most transformative technological shift in recent years has been the widespread adoption of telehealth. The COVID-19 pandemic significantly accelerated this trend, with telehealth appointments increasing by a staggering 154% during that period. This surge demonstrated the immense potential of virtual care to overcome geographic and mobility barriers. Patients in rural areas can now consult with specialists hundreds of miles away without leaving their homes. Individuals with mobility challenges can attend appointments without the arduous process of transportation and navigating inaccessible facilities.
Telehealth encompasses more than just video calls with a doctor. It includes Remote Patient Monitoring (RPM), where in-home technology tracks vital signs and other health data, transmitting it securely to healthcare providers. This empowers patients to take control of their health, reduces the need for frequent in-person visits, and can significantly lower rehospitalization rates. For those managing chronic conditions, RPM offers continuous oversight and proactive intervention, leading to better long-term health outcomes. These digital health tools are particularly beneficial for populations that traditionally struggle with access, such as the elderly, individuals with disabilities, and those in remote locations.
Ensuring Digital and Communication Accessibility
While technology offers incredible potential, its benefits can only be fully realized if it is designed with accessibility in mind. This means adhering to standards like the Web Content Accessibility Guidelines (WCAG) to ensure that digital health platforms, patient portals, and websites are usable by everyone, including those who rely on screen readers or other assistive technologies.
For effective communication, healthcare providers must leverage technology to bridge gaps. This includes offering Video Remote Interpreting (VRI) services for patients who are deaf or hard of hearing, ensuring they can communicate effectively with their medical team. For patients with cognitive or speech disabilities, digital communication aids and simplified interfaces can greatly improve their ability to engage with their care.
Here are key features for an accessible healthcare website:
- Clear and consistent navigation: Easy to understand and use for all.
- Keyboard navigability: All functions accessible without a mouse.
- Screen reader compatibility: Proper labeling and structure for assistive technologies.
- Adjustable text size and contrast: Options for users with low vision.
- Captions and transcripts for multimedia: For individuals with hearing impairments.
- Plain language: Easy-to-understand medical information.
- Error identification and suggestions: Helpful feedback for form completion.
By prioritizing digital and communication accessibility, we can ensure that technology truly serves as a bridge, not another barrier, in the pursuit of equitable healthcare.
Building an Inclusive System: Best Practices for Providers
For healthcare providers, moving towards a truly accessible system requires a comprehensive approach that goes beyond mere compliance. It demands a commitment to patient-centered care, robust staff training, and a deep understanding of legal requirements and disability etiquette.

Creating a Physically Accessible Environment
The foundation of accessible healthcare begins with the physical environment. Healthcare facilities must rigorously adhere to ADA (Americans with Disabilities Act) standards and Section 504 of the Rehabilitation Act, which mandate full and equal access for individuals with disabilities. This means ensuring:
- Accessible parking and pathways: Clear, wide routes from parking to entrances, free of obstructions.
- Ramps and wide doorways: Eliminating steps and ensuring entryways accommodate wheelchairs and other mobility devices.
- Accessible restrooms: Spacious stalls with grab bars, accessible sinks, and appropriate mirror heights.
- Clear internal navigation: Wide hallways, well-placed signage (including Braille and tactile text), and accessible elevators.
- Adjustable medical equipment: This is critical. As mentioned, only 40% of physicians often use accessible exam tables. Facilities should invest in height-adjustable exam tables, accessible scales, and mammography equipment that can accommodate patients using wheelchairs or with other mobility limitations. This not only ensures dignity for the patient but also reduces injury risk for both patients and staff.
Beyond general accessibility, specialized services must also consider their unique needs. For instance, services focusing on Rhode Island accessible men’s health must ensure their facilities and equipment are custom to the specific needs of men with various physical disabilities or conditions that might impact their ability to access care. This might include specialized privacy considerations or equipment designs. Regular accessibility audits, ideally involving individuals with disabilities, can help identify overlooked barriers and ensure continuous improvement.
Fostering Effective Communication and Trust
Physical accessibility is only one piece of the puzzle. Effective communication is equally vital for building trust and delivering quality care. Providers must adopt person-first language, recognizing that a person is not defined by their disability. Training staff on disability etiquette is crucial, ensuring they communicate directly with the patient, not just their companion or caregiver, and treat all patients with respect and dignity.
For patients with sensory disabilities, specific accommodations are necessary:
- Hearing disabilities: Provide qualified sign language interpreters when needed, use written notes for simpler exchanges, and ensure staff face the patient when speaking.
- Vision disabilities: Offer materials in large print, Braille, or electronic formats compatible with screen readers. Provide qualified readers if requested.
- Speech or cognitive disabilities: Practice patience, allow extra time for communication, repeat messages clearly, and use diagrams or pictures to aid understanding. Verify comprehension before moving on.
Building patient relationships also means addressing attitudinal barriers. This includes combating unconscious biases, avoiding assumptions about a patient’s capabilities or needs, and actively listening to their concerns. When patients feel heard, respected, and understood, they are more likely to engage with their care, leading to better health outcomes and a more positive healthcare experience.
The Broader Impact of Accessible Healthcare
The benefits of accessible healthcare extend far beyond the individual patient; they ripple throughout society, fostering stronger communities, improving public health, and contributing to economic stability.
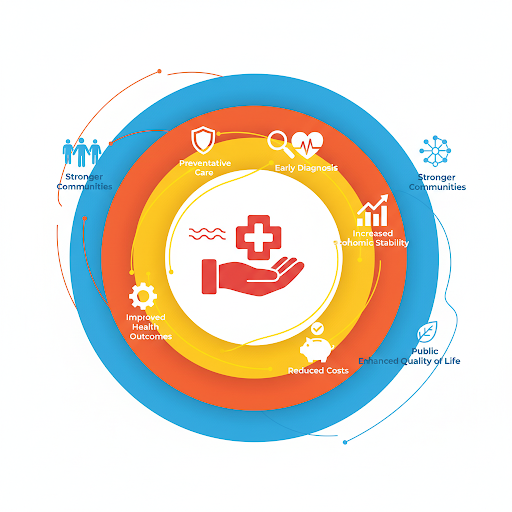
Health and Economic Benefits
When healthcare is easily accessible, individuals are more likely to seek preventative care and receive early diagnoses. This proactive approach can prevent minor health issues from escalating into severe, chronic conditions that require intensive and costly interventions. For example, regular screenings and timely treatment for conditions like diabetes or heart disease can significantly reduce the incidence of complications, improve quality of life, and extend healthy lifespans.
From an economic perspective, accessible healthcare leads to a healthier workforce, which in turn boosts productivity and reduces healthcare-related absenteeism. It also translates into lower long-term healthcare costs for individuals, families, and the healthcare system as a whole. When people can access primary care and preventive services, they are less likely to rely on expensive emergency room visits for manageable conditions. This reduction in emergency room use frees up critical resources for genuine emergencies. Furthermore, accessible care can reduce the financial strain on families, allowing them to allocate resources to other areas, strengthening the local economy.
Strengthening Communities Through Advocacy and Programs
Creating a truly accessible healthcare system is a shared responsibility that involves community health programs and robust advocacy efforts. Community health centers, mobile clinics, and health fairs play a vital role in bringing services directly to underserved populations, bridging gaps that traditional healthcare models often miss. These programs can offer screenings, vaccinations, health education, and basic medical care in convenient, familiar settings.
Policy advocacy is crucial for driving systemic change. This involves supporting legislation that mandates accessibility, increases funding for underserved areas, and expands insurance coverage. Advocacy groups, often led by individuals with disabilities and their allies, work tirelessly to raise awareness, challenge discriminatory practices, and ensure that the voices of those most affected are heard in policy debates.
Finally, empowering patients and involving people with disabilities in decision-making processes about their care and health-care policies is paramount. Their lived experiences provide invaluable insights into what truly works and what barriers still need to be overcome. By fostering these partnerships, we can co-create a healthcare system that is not only accessible but also truly patient-centered and responsive to the diverse needs of all members of our community.
Frequently Asked Questions about Healthcare Accessibility
What are the main legal requirements for healthcare providers?
Healthcare providers in the United States are primarily governed by two key federal laws regarding accessibility:
- The Americans with Disabilities Act (ADA): This civil rights law prohibits discrimination against individuals with disabilities in all areas of public life, including healthcare. Title II applies to state and local government entities (like public hospitals), while Title III applies to private entities operating places of public accommodation (like private clinics and hospitals). The ADA mandates both physical accessibility (e.g., ramps, wide doorways, accessible restrooms, adjustable medical equipment) and effective communication (e.g., qualified interpreters, accessible formats for information).
- Section 504 of the Rehabilitation Act: This law prohibits discrimination on the basis of disability by any program or activity receiving federal financial assistance. This includes many healthcare providers who accept Medicare or Medicaid. Section 504 has similar requirements to the ADA, ensuring that individuals with disabilities have full and equal access to services. Both laws aim to ensure that individuals with disabilities are not excluded from, denied the benefits of, or subjected to discrimination under any program or activity.
How can patients advocate for better access to care?
Patients play a crucial role in advocating for their own accessible healthcare and for broader systemic change. Here are some actionable steps:
- Know Your Rights: Familiarize yourself with the ADA and Section 504. Understanding what you are legally entitled to is your most powerful tool.
- Request Accommodations: Clearly communicate your needs when scheduling appointments. Don’t assume facilities will know what you require. Document these requests.
- Provide Feedback: If you encounter accessibility issues, respectfully inform the facility management. Suggest specific improvements. Your feedback is vital for change.
- Document Issues: Keep records of any accessibility barriers encountered, including dates, times, and specific details. This documentation can be helpful if further action is needed.
- Support Advocacy Organizations: Join or support local and national disability advocacy groups. These organizations work to influence policy and educate the public and providers.
- Communicate Clearly: During appointments, clearly state your communication preferences and needs to your healthcare team.
What is the first step a healthcare facility can take to become more accessible?
The most effective first step for any healthcare facility aiming to improve accessibility is to conduct a comprehensive self-assessment. This involves:
- Evaluating the Patient Journey: Map out the entire patient experience, from arrival (parking, entrance) through check-in, waiting areas, exam rooms, restrooms, and departure. Identify potential physical and communication barriers at each point.
- Physical Audit: Physically inspect the facility against ADA guidelines. Look for narrow doorways, lack of ramps, inaccessible restrooms, fixed-height exam tables, and other structural impediments.
- Communication Audit: Assess how information is provided and received. Are interpreters readily available? Are materials in accessible formats? Is the website compliant with WCAG?
- Staff Feedback: Engage staff from all departments. They often have knowledge of patient struggles and can offer valuable insights.
- Patient Input: Ideally, involve patients with diverse disabilities in this assessment. Their lived experiences are the most accurate indicators of true accessibility. Once barriers are identified, the facility can then prioritize changes based on legal mandates, patient impact, and available resources, creating a strategic plan for continuous improvement.
Conclusion
The journey toward truly accessible healthcare is ongoing, but it is a journey we are committed to. We have explored the significant barriers—financial, geographic, physical, and communicative—that prevent countless individuals from receiving the care they need. We’ve also highlighted how technology, particularly telehealth and remote monitoring, is bridging many of these gaps, bringing healthcare closer to home.
The responsibility for an inclusive system rests on the shoulders of healthcare providers, who must accept best practices in physical accessibility, effective communication, and patient-centered care. When we prioritize these efforts, the benefits are profound: improved public health, greater economic stability, and a higher quality of life for everyone.
Accessible healthcare is not a luxury; it is a fundamental right and a cornerstone of a compassionate society. It requires a universal commitment—from policymakers to providers, and from communities to individuals—to ensure that equitable medical services are a reality for all.

